COVID-19: THE CROWNED DOOM

Article by,

Dr. Binoy John, MD DM (CARDIOLOGY) FCSI FACC FESC FSCAI FAPSIC Senior consultant interventional cardiologist & specialist in heart failure & advanced cardiac diseases
A virus is not even a living thing, but yet has managed to get a technologically and militarily advanced human-world in its entirety into a stupefying and unimagined lock-down, while every other animal moves gracefully free! It is enigmatic to realize that this virus which is just 0.06 – 0.14 Microns in size and a mere structure of a single strand of nucleic acid, some lipids, proteins and carbohydrates and that which actually needs a host to propagate has humbled the scepter wielding powers of the world.
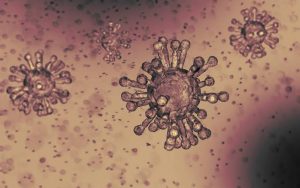
About the virus:
The Corona virus has spikes on it which gives it the appearance of a crown or corona, from which it derives its name. It is with these spikes that the virus gains entry into the host cells and multiplies and then causes all the ensuing destruction. It was initially named the novel corona virus and subsequently as the Severe Acute Respiratory Syndrome Corona Virus – 2 (SARS-CoV-2). The virus is presumed to have originated in bats and then moved to probably the pangolin before it infected the humans for the first time in Wuhan, Hubei province in China. The Corona Virus disease 2019 or the COVID-19, is now a global pandemic affecting over 3.2 million people and counting, in 210 countries and territories of the world.
How does the virus spread?
The virus is spread mainly via droplets but can be aerosolized when someone coughs or sneezes and can remain stable in the atmosphere for up to 3 hours in the aerosol, depending on factors such as atmospheric temperature, humidity and ventilation. It can remain on hard surfaces from 24 hours on cardboards and to as many as 3 days on steel and plastics. There are reports that the virus is excreted via the stools also. The virus has a high reproduction number and therefore spreads easily. So the common mode of infection is when a person with the virus contaminated hand touches the nose, mouth or eye or inhales the virus containing aerosol, with the virus thus gaining entry into the lungs.
The incubation time or the time between the entry of the virus into the body and appearance of symptoms is an average of 4 to 5 days, but can range from 1 to 14 days. An infected person can spread the virus even when he has no symptoms and thus be an asymptomatic carrier of the virus. It is the combination of the high infectivity along with the ability of a person to infect even when he is asymptomatic, that has been responsible for the rapid spread and the pandemic proportions of the disease.
How does it damage the lungs and other organs?
The primary target of the virus is the respiratory system and the virus uses its spike proteins to enter the lung cells by binding to a receptor called angiotensin converting enzyme 2 (ACE-2). This enzyme is expressed in the heart also, in addition to the lungs and also plays a key role in the functioning of the heart and development of high blood pressure in humans.
Once the virus enters the lungs it begins to multiply and the symptoms during these early stages are mostly mild or can be none at all. The protective mechanisms in the body tries to fight and suppress the virus by producing immune cells and also chemicals called cytokines. In some patients however, the release of these chemicals can be sudden and severely out of proportion, a phenomenon called, the ‘cytokine storm’ which ultimately turns out to be damaging to the patient himself. The chemical release damages the lungs causing breathing difficulty and the failure of lungs to oxygenate the blood results in decreased oxygen supply to all organs affecting their normal functioning too. When the kidneys start failing, the waste products start accumulating in the body, further depressing the function of the organs and also causes additional bacterial infection in the blood and organs causing septic organ failure.
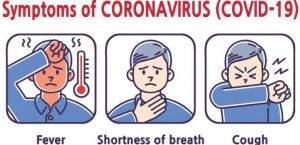
What are the symptoms and signs of COVID-19?
The usual symptoms are fever and dry cough but conspicuously a runny nose and gastrointestinal symptoms like diarrhea and vomiting are uncommon, though they can occur. 80% of the infected patients have no pneumonia (lung-infection) or may have only a mild pneumonia and only 15% develop more serious respiratory symptoms needing hospitalization and assisted breathing support and only 5% become critical with respiratory failure, shock and or multi organ failure.
Who are the people at high risk?
It is to be remembered that the virus is highly infective and all are equally susceptible to the infection. It is the severity of the disease and the complications that varies amongst subsets. The ones who are at risk for more severe disease, complications and a poorer outcome are people with poor immunity, the malnourished, elderly and frail, patients on long-term steroids and other immuno-suppressive drugs as liver, kidney and heart transplant patients.
COVID-19 and the heart:
The primary damage to the heart results from the lack of oxygen supply to the heart which causes a progressive failure in the pumping function of the heart. Added to this insult, the sudden chemical storm can cause a fall in the blood pressure which further reduces the blood and oxygen supply to the heart, thus creating a vicious cycle of increasing damage. The brain when it senses this poor pumping efficiency of the heart, in order to maintain adequate oxygen supply to the organs causes an increase in the heart-rate. This helps initially, but then the heart starts failing like a repeatedly flogged horse does, to a point when it cannot cope up further and a cardiac arrest ensues.
People with heart ailments are not especially prone for COVID-19 and their risk to get the infection is the same as any healthy person. However, patients with heart diseases can have more severe complications when they get COVID, especially those with previous heart-attacks, heart failure, children with certain cardiac birth defects (blue-baby defects) to mention a few. Pregnant women who have heart ailments may be at a higher risk too. However there is no evidence that the virus can infect implanted heart-devices like pacemakers or defibrillators or that it can directly infect the valves, muscle or the covering of the heart. However it is important to note that the stress on the heart produced by the chemical storm may cause rupture of fatty plaques or blocks inside the arteries of the heart and can cause a heart-attack.
Another point of controversy and debate is regarding two medications used commonly to treat high blood-pressure (Angiotensin converting enzyme inhibitors and Angiotensin II receptor blockers) which block ACE-2 and its system through which the virus enters the body. It was of concern that people taking these medications could develop more lung complications with COVID-19. However these observations have no confirmatory scientific evidence and major guideline forming cardiology societies and associations like the American Heart Association, European Society of Cardiology, and British Cardiac Society have recommended that these drugs should not be stopped, because these are drugs with proven benefits. Stopping cardiac medications without advice from the cardiologist can only lead to complications.
How deadly is COVID-19?
Thankfully, majority of the patients recover. The death rate from COVID 19 is estimated to be 1.4% (which for flu is only 0.1%). The fatality increases with increasing age being less than 1% for people less than 50 years 1.3% for 50 to 60 years, 3.6% for 60 – 70 years, 8% for 70 – 80 years and 15% for those above 80 years of age. Also death occurred only in 0.9% of the patients when there was no associated illnesses but it was 6 – 10% when the patients had associated high blood pressure, diabetes and other cardiac conditions. The reason or mechanism as to why patients with high blood pressure have higher death rates is unclear but could mostly be only an apparent association because of the higher prevalence of high blood pressure in elderly age group (> 70 years of age) which had maximum deaths.
Diagnosis of COVID-19:
Testing for COVID specifically relies mainly on three tests, the real time reverse transcription-polymerase chain reaction (RT-PCR) which is the gold-standard for SARS-CoV -2 viral genetic material, the antigen test which detects viral surface proteins (eg: spike protein) and the third being antibody (immunoglobulin) testing. RT-PCR and antigen tests use specimens collected from the respiratory tract secretions of the patient. All the tests are useful in different stages of the infection as their titres are variable with the duration of infection, viral load and severity of symptoms. False positive results can occur with antigen testing and false negative tests can occur if the specimen collection is improper. Therefore a negative test should be repeated in a patient in whom the clinical index of suspicion for COVID is high.
Antibodies are produced by blood cells called lymphocytes, specifically against the virus and the antibodies bind tightly to the virus to inactivate it. Antibody levels start rising with time as the body tries to fight the infection and blood samples are used for detection of these. The immunoglobulin (Ig) M antibodies are the first to be produced in response to the infection and Ig G starts rising a week to 10 days after onset of infection and remains in the blood even after the patient has recovered and is the one that indicates possible immunity from subsequent infections. But it is too early to say how much immunity would be conferred by Ig G antibodies against COVID-19.
Treatment of COVID-19:
Currently, the treatment is mainly supportive like ensuring control of fever, maintaining good hydration and nutrition and it is only when the oxygen content of the blood drops, the blood-pressure drops or the patient gets worse that hospitalization is advocated. Several drugs currently used against the virus are those targeted against the different mechanisms of virus multiplication and the chemical storm. An effective treatment or cure in the form of medications can only be obtained by a detailed understanding of the pathology of the disease obtained from post-mortem studies and a deep understanding of the microbiology of this novel virus, the pathogenesis and immunology of the disease and use of medications directed at every possible step. Until the recent evidence with the drug Remdesivir, there was no definitive success with the use of any specific drugs against the virus. All medications being used were merely on an experimental basis. However, Remdesivir an anti-viral drug which prevents multiplication of the virus in the body has been shown in a multi-centre randomized controlled trial to have clear-cut evidence in hastening the recovery of patients being treated with it. The use of Remdesivir has now been made ‘standard of care’ in the treatment of patients hospitalized with COVID-19.
Some of the other drugs being used in COVID-19 patients with variable results are those which would prevent virus entry into the cell (chloroquine) or to treat cytokine storm (Tocilizumab). Drugs like chloroquine and hydroxychloroquine have only been tested outside the human body to show some efficacy and there are no randomized controlled trials to prove its efficacy in humans with certainty. It is important however to remember that some of the drugs have cardiac side effects and can cause electrical abnormalities called ‘torsades de pointes’ which can cause sudden cardiac death and therefore needs electrocardiogram (ECG) monitoring and should not be taken without consulting a specialist.
Treatment with convalescent plasma is another option being investigated and attempted. It involves the transfusion of plasma obtained from recovered patients, containing high titres of antibodies against SARS Co V- 2, into other patients who have less severe infection or patients who are in early stages of the infection or people who are at high risk of getting COVID, as health-care professionals. The antibodies present will prevent multiplication of the virus in the body and thus prevent lung and other organ damage. However this procedure is not totally risk free to the person receiving the treatment and have a risk of transmitting other infections and causing other immune reactions.

Prevention is better than cure:
As of now with no cure in hand, prevention is the key and the steps to prevention are simple and involves avoiding touching the mouth, nose and eyes with unclean hands, washing hands thoroughly with soap and water for at least twenty seconds or the use of hand-sanitizers containing at least 60% alcohol. It is also important to keep frequently touched objects clean with disinfectants. Practicing social distancing or maintaining a safe distance of at least two metres from other people whenever possible and keeping away from sick people even if their symptoms are mild and also staying away from crowded areas is vital. Also covering one’s nose and mouth with a cloth or with the inside of the elbow when one sneezes or coughs and using the non-dominant hand to touch objects so that you would not unknowingly use it to touch your mouth nose or eyes are good practices. Wearing the right protective masks in public places is crucial and only masks which are recommended for COVID-19 protection will be protective and have to be used in the right manner and will be useful in public places where the chances of getting infected are high.
If one experiences fever, cough or chest infection it is important to consult a doctor on the phone and follow his instructions and get tested only after taking professional advice as testing centres can be potential areas of high infectivity.
Vaccines and immunity:
Vaccines are being researched on fervently but would take a while to be available for human use, after they are tested in animals and proven to be effective and safe. After the first infection, it is speculated that COVID 19 would confer immunity but if mutations and fresh strains occur, they could re-infect, and would need fresh vaccines, information about which is currently unavailable. Herd immunity is a concept where, when a large percentage of the population are infected and recover and get immunity, thereby providing protection in a community, where the chances of non-immune people getting infected are less because the percentage of infected carriers in that community steadily becomes fewer.
Thus, the COVID-19 has taken an erstwhile head-strong and free world unawares, with a chilling shock, sending them into hiding, when an invisible nothing has humbled seemingly invincible powers and the powerful of the world, putting medical researchers and organizations on their toes desperately trying to find a quick resolve, while the front-liners strive tirelessly risking their own lives to save humanity from a rapidly decimating disease. Adding to the cost of life, the economic repercussions would be severe too.
This infliction of unimaginable proportions has also given humanity an opportunity to introspect on the wrongs we have committed, when we abused nature with all our power and glory; has given us a time to introspect on what we did wrong as a world and as individuals when we divided ourselves with borders, languages, colour, religions, caste and what not; when now, standing together singularly as humanity with humaneness seems to be the only way to tide over this catastrophe of unfathomable proportions. Let us change for the better, but then will we be given that chance? Hope and faith is what has always kept the world going and so may God bless us all!
Pic Courtesy: google/ images are subject to copyright